Melanoma is the most aggressive and deadliest form of skin cancer. Effective treatments are elusive because one type of this cancer develops resistance to available inhibitors, and in another type, no effective drug treatment has yet been found.
But a promising pathway to effective drug treatment of both types of melanoma has been identified by Cornell researchers in the signal regulating protein PLEKHA4, found in numerous animal tissues and organs, including the skin.
Melanoma stopped growing in tumor cells where PLEKHA4 was removed absent, the researchers found, making this protein a likely target for anti-cancer therapies. The results appear in “PLEKHA4 promotes Wnt/β-catenin signaling-mediated G1-S transition and proliferation in melanoma,” published in Cancer Research Feb. 11.
The study identifies PLEKHA4 as a promising drug target for melanoma, said corresponding author Jeremy Baskin, assistant professor of chemistry and chemical biology in the College of Arts and Sciences. The study also confirms that Wnt/beta-catenin signaling, a process with known connections to colorectal cancer, is connected to melanoma, as well.
In 2019, Baskin and collaborators published their discovery of how PLEKHA4 prepares a cell to respond to Wnt signaling – a process that tells a cell to divide, to move to a different part of the body, or to differentiate into a new kind of cell. PLEKHA4 is a regulator in this process, controlling how strongly a Wnt pathway signals in a cell.
“In healthy cell development, PLEKHA4 can control proliferation but also differentiation – a cell changing its identity when dividing,” said Baskin, who also has an appointment in the Weill Institute for Cell and Molecular Biology.
This protein is therefore important in Wnt signaling in animal embryos and also in adult systems that require frequent cell replacement, such as the digestive tract.
“If I were a cancer, I would want to co-opt Wnt signaling because it’s a pathway the body already has for telling cells to divide,” Baskin said.
Adnan Shami Shah, doctoral student and lead author of the paper, observed that cancer cells depleted of PLEKHA4 proliferated more slowly than cells that had the protein, Baskin said. Shami Shah then focused specifically on melanoma cells, in which PLEKHA4 is present at the highest levels relative to cells from other types of cancer.
“When he cultured melanoma cells and depleted the protein, they flatlined. It was a very strong effect,” Baskin said.
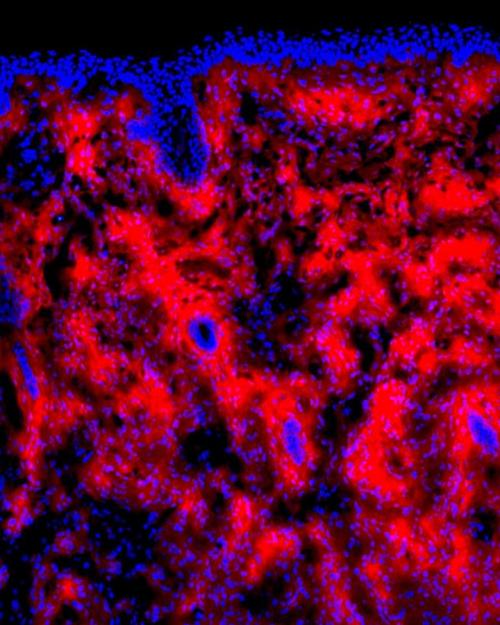
The team conducted a series of experiments on different types of melanoma cells in cell culture, investigating whether removing PLEKHA4 using RNA interference would decrease proliferation of the cancer cells. They finished the study with mouse models of melanoma in collaboration with Andrew C. White, assistant professor of biomedical sciences in the College of Veterinary Medicine, a co-author. The study was also co-authored by doctoral student Xiaofu Cao.
“We found that once the tumors had the protein [PLEKHA4] removed, they stopped growing,” Baskin said.
The researchers found that depleting PLEKHA4 had a strong effect on proliferation in two types of melanoma: BRAF-mutant, the treatments for which lead to resistance; and NRAS-mutant, which has no current targeted therapy treatments.
“We think that if we could develop a drug that could inhibit PLEKHA4, it might work in both those types of melanomas,” Baskin said.
Moreover, the researchers found that depleting PLEKHA4 in the presence of an existing inhibitor of BRAF-mutant melanoma made the tumors get even smaller than either alone – it had an additive effect, Baskin said: “That was exciting because typically when a new drug is developed for a disease where the difference is life and death, you don’t take away the existing treatment; you add it to the standard of care.”
Baskin said he is excited about this potential pathway for treating melanoma, which is dangerous because of its ability to spread from skin to other tissues.
“Cancer is uncontrolled cell growth and division, and the tumors work hard to get around the drugs,” Baskin said. “We always need new pathways to target so we can develop new therapies that can work alone or in combination with existing ones.”
This research received support from the National Institutes of Health and the Alfred P. Sloan Foundation.